ACL Reconstruction
What is Your Anterior Cruciate Ligament (ACL)?
The anterior cruciate ligament is one of the major stabilizing ligaments in the knee. It is a strong rope- like structure located in the center of the knee running from the femur to the tibia.
When this ligament tears unfortunately, it doesn't heal and often leads to the feeling of instability in the knee.
ACL reconstruction is a commonly performed surgical procedure and with recent advances in arthroscopic surgery can now be performed with minimal incisions and low complication rates.
What Does the ACL Do?
The ACL is the major stabilizing ligament in the knee. It prevents the tibia (shin bone) moving abnormally on the femur (thigh bone). When this abnormal movement occurs, it is referred to as instability and the patient is aware of this abnormal movement.
Often, other structures such as the meniscus, the articular cartilage (lining the joint) or other ligaments can also be damaged at the same time as a cruciate injury and these may need to be addressed at the time of surgery.
- Most injuries are sports-related involving a twisting injury to the knee.
- It can occur with a sudden change of direction, a direct blow, e.g., a tackle, landing awkwardly.
- Often there is a popping sound when the ligament ruptures.
- Swelling usually occurs within hours.
- There is often the feeling of the knee popping out of joint.
- It is rare to be able to continue playing sport with the initial injury.
Once the initial injury settles down, the main symptom is instability or giving way of the knee. This usually occurs with running activities, but can occur with simple walking or other activities of daily living.
The diagnosis can often be made on the history alone.
Examination reveals instability of the knee, if adequately relaxed or not too painful.
An MRI (Magnetic Resonance Imaging) can be helpful if there is a doubt, or to look for damage to other structures within the knee.
At times the final diagnosis can only be made under an anesthetic or with an arthroscopy.
What are the Treatment Options?
Initial
- Rest
- Ice
- Elevation
- Bandage
Long Term
Not everyone needs surgery. Some people can compensate for the injured ligament with strengthening exercises or a brace.
It is strongly advised to give up sports involving twisting activities, if you have an ACL injury.
- Episodes of instability can cause further damage to important structures within the knee that may result in early arthritis
What are the Indications for ACL Surgery?
Young patients wishing to maintain an active lifestyle.
Sports involving twisting activities, e.g., soccer, netball, football Giving way with activities of daily living.
People with dangerous occupations, e.g., policemen, firemen, roofers, scaffolders.
It is advisable to have physiotherapy prior to surgery to regain motion and strengthen the muscles as much as possible.
How is and ACL Reconstruction Performed?
Surgical techniques have improved significantly over the last decade, complications are reduced and recovery much quicker than in the past.
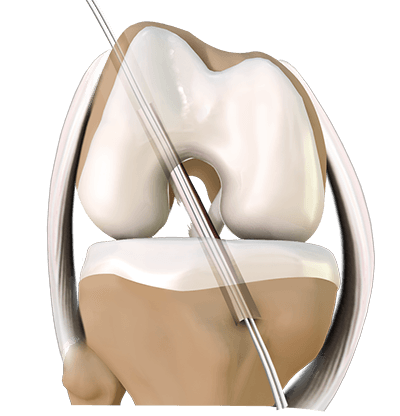
The surgery is performed arthroscopically. The ruptured ligament is removed and then tunnels (holes) in the bone are drilled to accept the new graft. This graft which replaces your old ACL is taken either from the hamstring tendon ( or an artificial ligament is used). DR Graham will discuss these options with you prior to surgery.
The graft is prepared to take the form of a new tendon and passed through the drill holes in the bone.
The new tendon is then fixed into the bone with various devices to hold it in place, while the ligament heals into the bone (usually 6 months).
The rest of the knee can be clearly visualized at the same time and any other damage is dealt with, e.g meniscal tears.
The wounds are then closed and a dressing applied.
What do the Post-operative Steps Include?
Surgery is performed as a day procedure or an overnight stay.
- You will have pain medication by tablet or in a drip (intravenous).
- A splint is sometimes used for comfort.
You will be seen by a Physiotherapist who will teach you to use crutches and show you some simple exercises to do at home.
Leave any waterproof dressings on your knee until your post-op review.
You can put all your weight on your leg.
Avoid any anti-inflammatory or aspirin for 10 days.
Put ice on the knee for 20 minutes at a time, as frequently as possible.
Post-op review will usually be after 10-14 days.
Physiotherapy can begin after a few days or can be arranged at your first post-op visit.
If you have any redness around the wound or increasing pain in the knee or you have a temperature or feel unwell, you should contact Dr Graham's office or your GP as soon as possible.
Why is Rehabilitation for ACL Reconstruction Essential?
Physiotherapy is an integral part of the treatment and is recommended to start as early as possible. Pre-operative physiotherapy is helpful to better prepare the knee for surgery. The early aim is to regain range of motion, reduce swelling and achieve full weight-bearing.
The remaining rehabilitation will be supervised by a Physiotherapist and will involve activities such as exercise bike riding, swimming, proprioceptive exercises and muscle strengthening. Cycling can begin at 2 months, jogging can generally begin at around 3 months. The graft is strong enough to allow sport at around 6 months. However, other factors come into play such as confidence, fitness and adequate training.
Professional sportsmen often return at 6 months but recreational athletes may take 10 -12 months depending on motivation and time put into rehabilitation.
The rehabilitation and overall success of the procedure can be affected by associated injuries to the knee such as damage to meniscus, articular cartilage or other ligaments.
The following is a more detailed rehabilitation protocol useful for patients and physiotherapists. It is a guide only and must be adjusted on an individual basis taking into account pain, other pathology, work and other social factors.
Please refer to post operative download section for the full rehabilitation program.
ACL Reconstruction Rehabilitation Program
Day 1-14
Aims
- reduce post-operative pain, control effusion and minimise effects of surgery on soft tissue.
- restore normal gait.
Goals
- reduce joint effusion
- prevent infection / facilitate wound healing
- re-establish muscle activation
- restore full extension
- manage donor site morbidity
Treatment Strategies
- partial weight-bearing to full weight bearing as tolerated
- use of ICE, co-contractions and external pressure support to control pain swelling
- static quads, co-contraction (progressing into weight-bearing positions)
NB - quadriceps exercises are to be closed kinetic chain - active range of motion aiming for full extension by two weeks post-surgery.
- prevent secondary patello-femoral joint problems (patellar mobilisation, myofascial releases ITB etc)
- retrain full extension at heel strike
- gentle hamstring stretches
2-6 Weeks
Aim
Restore normal function.
Goal
- full unrestricted ROM
- reduce persistent effusion
- early proprioceptive retraining
- develop muscle control and endurance
Treatment Strategies
- 2-3 weeks - improve muscular control by progressing co-contractions
eg; two leg quarter squats, step ups and lunges - introduce stationary bike, stepper and leg presses as tolerated (do not start these activities until any persistent effusion settles)
- Swimming once wound has healed
- 3-4 weeks - initially hamstring strengthening is achieved via co-contraction (closed kinetic chain). It is important to concentrate on hamstring stretches and increase resistance gradually to prevent recurrent injury.
4-6 weeks - open kinetic chain hamstring strengthening may begin but care must be taken to avoid strain injury as it impedes progress. Low resistance, high repetition weights to increase muscle endurance. - assessment and monitoring of gluteal control and length of hamstrings. ITB, gastrocs and soleus, etc will prevent secondary deficits from developing
6-12 Weeks
Aim
Improve proprioception.
Goals
- improve endurance of leg musculature
- increase total leg strength
Treatment Strategies
- progress general strength work
- hopping and jumping introduced into proprioceptive retraining (focus on good landing technique)
- agility work (shuffle runs, ball skills, sideways running, skipping ropes etc)
- pool work may commence with flippers
- sports specific activity (sport dependent)
12 Weeks - 6 Months
Aim
Prepare to return to sport.
Goals
- introduce more sport specific activities
- develop patina confidence
- introduce agility and reaction time into proprioception work
Treatment Strategies
- progress general strength work
- hopping and jumping introduced into proprioceptive retraining (focus on good landing technique)
- agility work (shuffle runs, ball skills, sideways running, skipping ropes etc)
- pool work may commence with flippers
- sports specific activity (sport dependent)
5-6 Months
Goals
Return to sport safely.
Treatment Strategies
- open kinetic quadriceps exercises can be done safely
- introducepolymetrics and sport specific drills
- return to training and participating in skill exercises
- improve power and endurance
- advice re: modification for gradual return to sport
What are the Risks & Complications for ACL Reconstruction?
Complications are not common but can occur. Prior to making the decision to have this operation, it is important you understand these so you can make an informed decision on the advantages and disadvantages of surgery.
These can be medical (Anesthetic) complications and surgical complications.
Summary
Anterior Cruciate Ligament reconstruction is a common and very successful procedure. Dr Edward Graham performs a lot of these procedures, 95% of people have a successful result. It is generally recommended in the patient wishing to return to an active lifestyle, especially those wishing to play sports involving running and twisting.
The above information hopefully has educated you on the choices available to you. If you have any further questions you should consult with Dr Graham and his Staff.
Treatment Process
Preparation for Surgery
- Provide a complete list of your medications so you can be advises which to stopped prior to surgery,
- Treat any tooth, gum, bladder or bowel problems before surgery to reduce the risk of infection
- Stop anti-inflammatory medications (NSAIDs) at least seven days before the procedure.
- Stop or cut down smoking to reduce your surgery risks and improve your recovery
- Consider losing weight (if overweight) before surgery
Day of Surgery
- Report any infections to me prior to surgery as the procedure cannot be performed until all infections have cleared up.
- Do not consume alcohol - 24 hours prior to treatment,
- Do not eat or drink anything, including water, for 6 hours before surgery
- Avoid vigorous physical activity or exercise 24 hours prior to surgery,
During Surgery
- Administration of general anesthesia or sedation and local anesthesia
- The entire procedure can take 60 minutes to two hours.
- Procedure is performed and sent to recovery room, for observation
- Pain medications are prescribed to help with pain during the recovery phase.
After Surgery
- Do not consume large amounts of alcohol after surgery,
- Avoid vigorous physical activity or exercise until advised,
- Follow the Post Surgery Treatment Plan proscribed by the surgeon and post op care specialists.
- Any questions or complications should be communicated directly to the surgeon